As an obstetrician-gynecologist who has walked thousands of patients through their nine-month journey, I know that pregnancy isn’t always a glowing experience. It often comes with real aches, pains, headaches, and fevers. When a splitting migraine hits or your lower back feels like it’s giving out, your first instinct is probably to reach for the medicine cabinet.
Before you were pregnant, popping an Advil or Motrin was likely a second thought. Now, everything you put in your body raises a question: “Is this safe for my baby?”
This is one of the most frequent questions I get in my clinic. It is also one of the most important to answer correctly because the guidance on pain relief has changed significantly over the years due to better research and stricter warnings from health organizations like the FDA.
Here at PregnancyClarity, my goal is to cut through the noise of internet forums and give you straight medical facts delivered with the same care I give my own patients. Let’s break down exactly why ibuprofen is generally off-limits during pregnancy and what you can do instead to manage pain safely.
Is Ibuprofen Safe While Expecting? The Direct Answer
If you are looking for a quick “yes” or “no,” the answer is generally no. You should avoid taking ibuprofen during pregnancy unless a doctor specifically tells you it is necessary for a unique medical situation.
Ibuprofen belongs to a class of drugs called Nonsteroidal Anti-Inflammatory Drugs, or NSAIDs. Other common drugs in this category include aspirin and naproxen (Aleve). These drugs work by blocking certain enzymes in your body that create prostaglandins, chemicals that cause pain, fever, and inflammation.
While reducing inflammation is great for a sprained ankle when you aren’t pregnant, those same prostaglandins play vital roles in fetal development. Messing with their production while a baby is growing can lead to unintended consequences. The risks change depending on how far along you are, but the safest route is to keep the bottle closed until after delivery.
Risks of Taking Ibuprofen in Each Trimester
Pregnancy is a dynamic process, and the baby’s vulnerability to certain medications changes as their organs develop. The risks associated with NSAIDs like ibuprofen are different at week 8 than they are at week 28.
First Trimester: Miscarriage and Development Concerns
The first twelve weeks are a period of rapid development. The baby’s major organ systems are just forming.
Some research suggests that taking NSAIDs around the time of conception or in early pregnancy might be linked to a slightly higher risk of miscarriage or certain birth defects, particularly those involving the heart or abdominal wall.
While the data on first-trimester use isn’t as definitive as later stages, most gynecologists, myself included, prefer to err on the side of caution. There are safer alternatives available that don’t carry these potential risks during such a sensitive developmental window. If you are experiencing unusual cramping or spotting or bleeding early on, it is always best to consult your doctor rather than trying to self-medicate with ibuprofen.
The Second Trimester: The FDA’s 20-Week Warning
For a long time, the medical community viewed the second trimester as a relatively “safe” zone for occasional NSAID use. That changed significantly a few years ago.
The U.S. Food and Drug Administration (FDA) issued a strong warning advising against the use of NSAIDs beginning around 20 weeks of pregnancy. This is because around the midpoint of pregnancy, the baby’s kidneys become the primary producer of amniotic fluid.
Taking ibuprofen during this phase can reduce blood flow to the baby’s kidneys. If their kidneys aren’t working fully, they don’t produce enough urine. Since fetal urine makes up most of the amniotic fluid, fluid levels can drop dangerously low.
The Third Trimester: Serious Risks to the Baby’s Heart
Once you reach the third trimester (around 28 weeks), the warning against ibuprofen becomes even stricter. Taking NSAIDs late in pregnancy can cause serious, sometimes permanent, problems with the baby’s heart and blood circulation.
This is practically a universal rule among obstetricians: do not take ibuprofen in the third trimester. The risks to the baby’s cardiovascular system are too high.
Specific Dangers: How Ibuprofen Affects Your Baby
To truly understand why we are so cautious, it helps to know a little bit about fetal physiology. Ibuprofen doesn’t just “hurt” the baby; it interferes with specific mechanisms the baby needs to survive inside the womb.
Low Amniotic Fluid (Oligohydramnios)
As mentioned regarding the FDA warning, amniotic fluid isn’t just water. It’s mostly baby urine. This fluid is essential because it provides a cushion for the baby, protects the umbilical cord from being compressed, and helps the baby’s lungs develop as they “breathe” the fluid in and out.
When ibuprofen restricts blood flow to fetal kidneys, urine output drops, and amniotic fluid levels decrease. This condition is called oligohydramnios. Low fluid can lead to poor lung development and joint contractures because the baby doesn’t have enough room to move.
Fetal Heart Complications (Ductus Arteriosus)
This is the most significant worry in the third trimester. Every fetus has a special blood vessel near their heart called the ductus arteriosus. Before birth, the baby doesn’t use their lungs to get oxygen; they get it from the mother via the placenta. The ductus arteriosus allows blood to bypass the fluid-filled lungs, sending oxygenated blood directly to the body.
This vessel is supposed to stay open until the baby takes their first breaths after birth. Prostaglandins—the exact chemicals ibuprofen blocks, are what keep this vessel open inside the womb.
If you take ibuprofen late in pregnancy, it can cause this vessel to close prematurely while the baby is still inside you. This can lead to high blood pressure in the baby’s lungs, a serious condition known as Persistent Pulmonary Hypertension of the Newborn (PPHN).
Safe Alternatives for Pain Relief During Pregnancy
Just because you can’t take ibuprofen doesn’t mean you have to suffer through pain. Pregnancy is hard on the body, and we want you to be comfortable.
Why Acetaminophen (Tylenol) is the Standard Choice
When patients ask about pain relief, acetaminophen (Tylenol) is almost always the recommended first-line option.
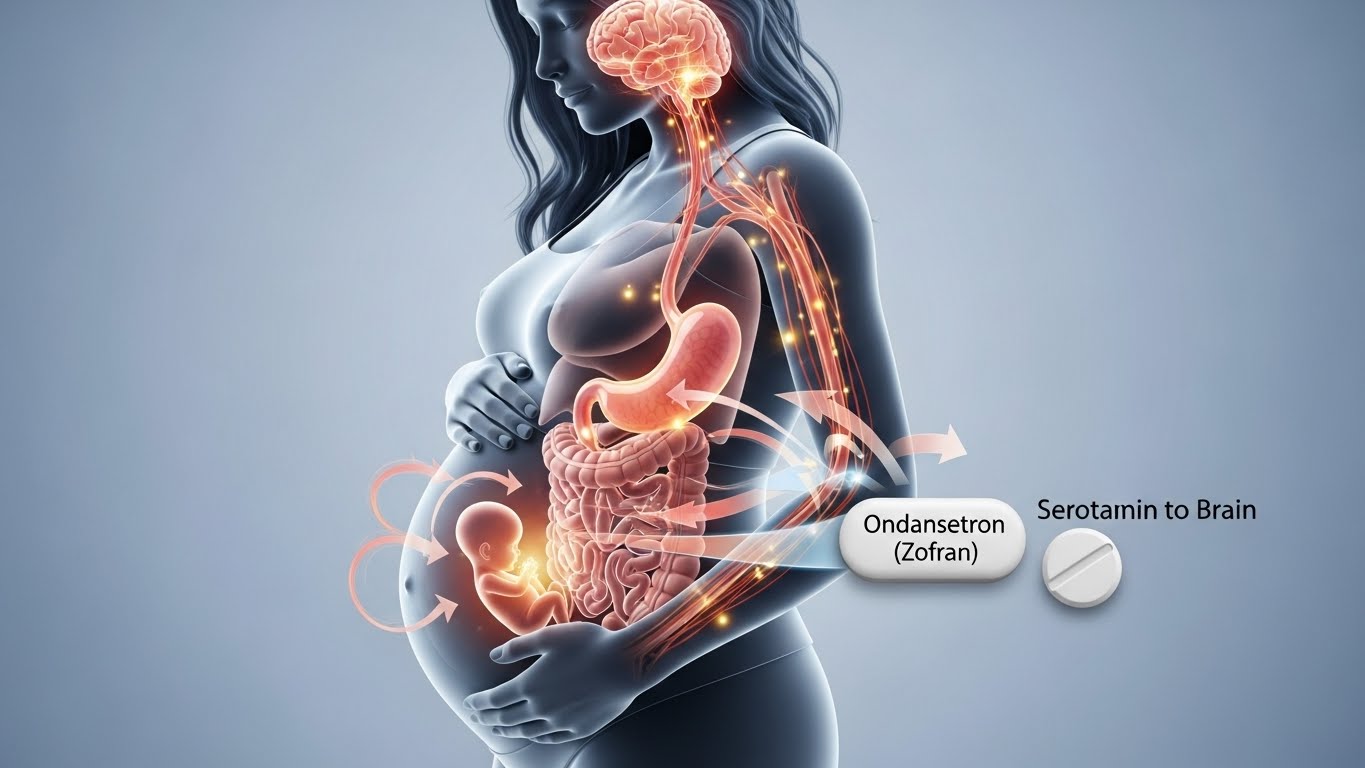
Unlike ibuprofen, acetaminophen is not an NSAID. It works differently in the brain to reduce pain and fever and does not have the same effects on fetal kidneys or heart vessels. Decades of use have shown it to be the safest choice for pain relief during all stages of pregnancy when taken according to the dosage instructions on the bottle.
Of course, even with “safe” drugs, the goal is always to take the lowest effective dose for the shortest amount of time necessary. If you are unsure about any over-the-counter drug, it’s always worth checking our guide on safe medications during pregnancy.
Drug-Free Ways to Manage Aches and Pains
Often, mechanical pain—like backaches or round ligament pain, responds better to physical changes than to pills.
- Heat and Cold: A warm heating pad (on a low setting, not directly on the belly) can work wonders for back pain. Ice packs can help with tension headaches.
- Support Gear: Belly bands can help lift the weight of your growing uterus off your hips and lower back.
- Physical Therapy or Massage: Seeing a physical therapist who specializes in pregnancy or getting a prenatal massage can provide significant relief for musculoskeletal pain.
- Hydration: Dehydration is a very common trigger for headaches and uterine cramping during pregnancy.
Common Questions About Ibuprofen and Pregnancy
What if I took ibuprofen before I knew I was pregnant?
Don’t panic. This happens frequently. Many women take ibuprofen for period cramps just before realizing they missed their period.
The risk from a few doses taken in the very first few weeks after conception is generally considered low. The “all-or-nothing” concept often applies here—either the pregnancy continues normally, or it doesn’t implant. If you have a positive pregnancy test and took ibuprofen last week, stop taking it now and start taking your prenatal vitamins. Mention it to your doctor at your first appointment for peace of mind, but try not to worry.
Are topical ibuprofen gels safe to use?
Some people think creams or gels applied to the skin are safer because you aren’t swallowing a pill. While it is true that less of the drug reaches your bloodstream compared to oral tablets, some is still absorbed.
Because we want to avoid any NSAID exposure to the fetus, most obstetricians recommend against using topical ibuprofen gels (like Voltaren) as well, especially in the later stages of pregnancy. Stick to topical creams that use menthol or capsaicin if you need localized relief, but check with your provider first.
Is a single dose of Advil or Motrin dangerous?
If you took one pill by accident because you had a blinding headache, it is highly unlikely to cause permanent harm to your baby, especially if it wasn’t in the third trimester. The severe risks like kidney issues and heart vessel closure are usually associated with regular, repeated use for days or weeks.
However, because we can’t ethically test “how much is too much” on pregnant women, we don’t know the exact safe threshold. That is why the advice is to avoid it entirely. If you took a dose by mistake, don’t beat yourself up, just switch to acetaminophen next time.
Final Safety Checklist for PregnancyClarity Readers
Navigating pregnancy requires making hundreds of small decisions for the health of your baby. We want the PregnancyClarity community to feel empowered by facts, not overwhelmed by fear.
When it comes to pain:
- Avoid Ibuprofen (Advil, Motrin) and other NSAIDs like naproxen (Aleve) throughout pregnancy, but especially after 20 weeks.
- Choose Acetaminophen (Tylenol) if you need medication for pain or fever.
- Try non-drug methods first, such as rest, hydration, heating pads, or stretching.
- Talk to your OB-GYN before starting any new medication, even over-the-counter ones.
If you are in severe pain that isn’t helped by Tylenol, or if you have serious early pregnancy symptoms, don’t just tough it out at home. Call your doctor. We are here to help you manage the discomfort safely so you can focus on preparing to meet your new baby.