As a gynecologist, I see the look of worry on a patient’s face the moment I mention the word “antibiotic.” If you are currently pregnant and have been handed a prescription for Metronidazole, also known by the brand name Flagyl, it is completely normal to feel a bit uneasy. You want what is best for your baby, and the idea of putting a strong medication into your body can feel like a risk.
At PregnancyClarity, we aim to strip away the confusion and give you the medical facts mixed with real-world clinical experience. So, is Metronidazole safe during pregnancy? The short answer is yes, in most cases, it is considered safe and often necessary. However, the timing of when you take it and the reason for the prescription matter quite a bit.
What is Metronidazole and Why Do You Need It?
Metronidazole is a specific type of antibiotic that targets “anaerobic” bacteria and certain parasites. These are organisms that thrive in environments without much oxygen, like the vaginal canal or the gut.
In my practice, I most commonly prescribe this for two reasons: Bacterial Vaginosis (BV) and Trichomoniasis. While these might seem like “annoying” infections rather than serious medical emergencies, they carry significant risks when you are pregnant. Untreated BV, for instance, is linked to a higher chance of your water breaking too early (preterm rupture of membranes) or the baby being born before they are fully ready.
The Trimester Breakdown: When Is It Safest?
The most common question I get in the exam room is: “Will this hurt my baby’s development?” To answer this, we look at the trimesters.
The First Trimester: A Season of Caution
During the first 13 weeks of pregnancy, the baby is undergoing “organogenesis.” This is the critical window where the heart, lungs, and limbs are forming. Historically, some doctors were hesitant to use oral Metronidazole during this time because of older animal studies that suggested potential risks.
However, modern medical consensus from the CDC and the American College of Obstetricians and Gynecologists (ACOG) has found no clear evidence that Metronidazole causes birth defects in humans. That said, if your infection is mild, many doctors (including myself) might suggest waiting until the second trimester or using a vaginal gel instead of an oral pill to limit how much of the medicine enters your bloodstream.
The Second and Third Trimesters: Standard Treatment
Once you enter the second trimester, the “safety profile” of Metronidazole becomes much clearer. By this stage, the baby’s major structures are formed. The focus shifts to maintaining a healthy environment for the baby to grow. Treating a vaginal infection now is actually a protective measure. Most clinical data shows that taking the full course of Metronidazole in the later stages of pregnancy does not increase the risk of low birth weight or other complications.
Why Treating the Infection is Often Safer Than Doing Nothing
It is easy to think that “natural is better” and that your body will fight off the infection on its own. While that is true for some minor issues, bacterial infections in the reproductive tract are different.
When you have BV, the balance of “good” bacteria (Lactobacilli) is replaced by “bad” bacteria. This can lead to inflammation. This inflammation can weaken the amniotic sac or even trigger early contractions. In my years of experience, I have seen more complications arise from untreated infections than from the antibiotics used to cure them.
If you are dealing with pelvic pain or discomfort along with the infection, you might be tempted to reach for your usual pain relievers. However, it is vital to be careful here. While you are working on clearing up the infection, remember that avoiding ibuprofen is a standard rule for most of pregnancy, as it can affect the baby’s heart and kidney development. Stick to Tylenol (acetaminophen) unless your doctor tells you otherwise.
Common Side Effects and How to Handle Them
If you start taking Metronidazole, you will likely notice a few things. First, the “metallic taste” is real. Many women describe it as having a penny under their tongue. This is harmless but annoying.
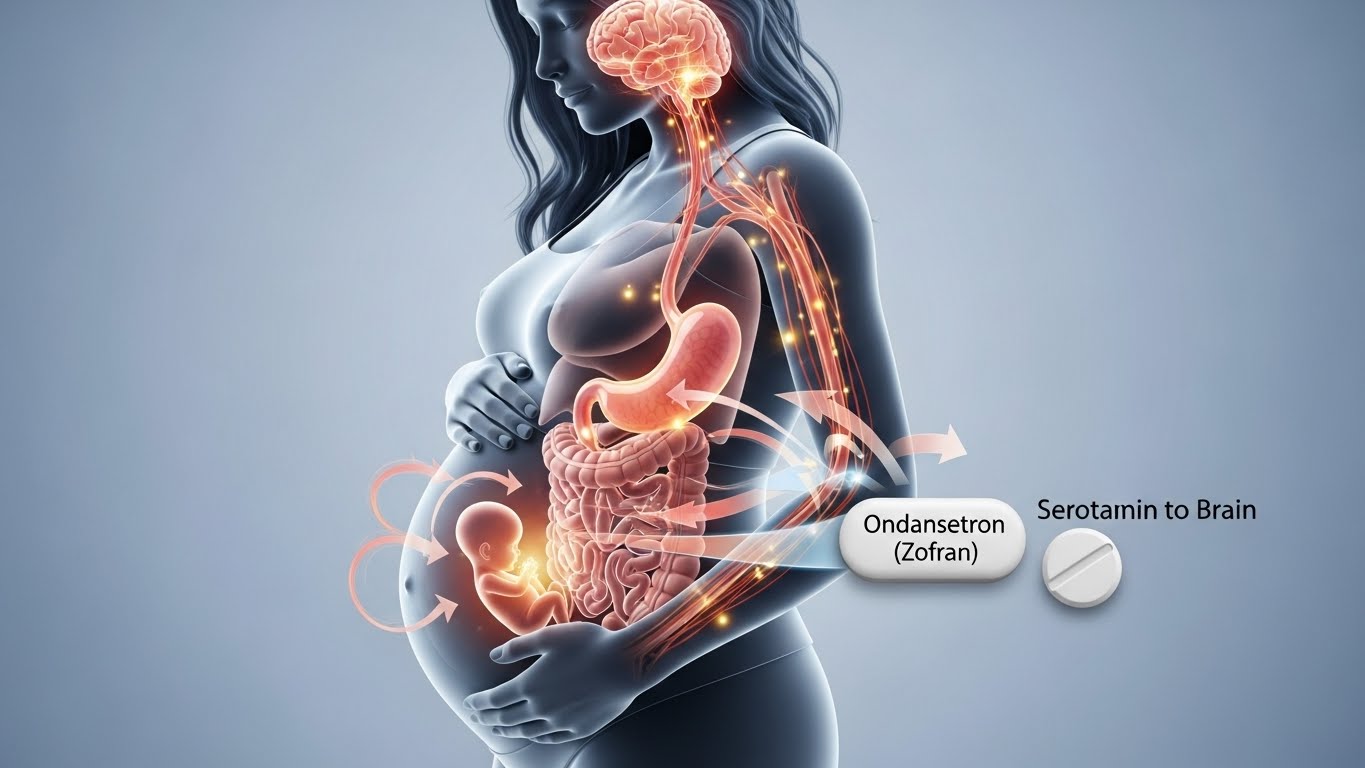
Second, this medication can be tough on the stomach. Nausea is a frequent complaint. If the antibiotic is making you feel sick to your stomach, it can be hard to tell if it’s the medicine or just standard pregnancy symptoms. For those who are already struggling with morning sickness, we often look for ways to manage the stomach upset. In severe cases, your doctor might discuss options for safely managing morning sickness with Zofran to help you keep the necessary antibiotics down.
The “No Alcohol” Rule
This is the most important “tip” I can give you. Metronidazole causes a very unpleasant reaction if you consume even a tiny amount of alcohol. It can lead to severe vomiting, a racing heart, and a flushing face. While most pregnant women aren’t drinking anyway, be sure to check your mouthwash or any herbal tinctures you might be using to ensure they are alcohol-free while you are on this medication.
Oral Tablets vs. Vaginal Gel
Your doctor may give you a choice between taking a pill or using a vaginal cream (Metrogel).
- Oral Tablets: These are usually more effective for treating Trichomoniasis because the infection can sometimes hide in the urinary tract where a cream can’t reach.
- Vaginal Gel: This is often the preferred choice for BV in pregnancy because only a small amount of the medication is absorbed into your body. It works directly where the problem is.
If you find that the oral pills are causing too much heartburn or “acid reflux,” you aren’t alone. Pregnancy hormones already slow down your digestion, making heartburn more common. If you need safe acid reflux relief, Pepcid is a common recommendation that can help settle that burning sensation while you finish your antibiotic course.
A Note on Probiotics and Recovery
Antibiotics are like a “reset button” for your bacteria, they kill the bad stuff, but they can also take out some of the good stuff. After you finish your prescription, I often recommend that my patients eat yogurt with live cultures or take a high-quality prenatal probiotic. This helps restore the healthy bacteria in your gut and vagina, which can prevent a yeast infection from following right on the heels of your BV treatment.
Final Thoughts from the Clinic
At the end of the day, your healthcare provider has weighed the risks and benefits before writing that script. If you are diagnosed with a symptomatic infection, taking the Metronidazole is almost always the right move for both you and your baby.
We created PregnancyClarity to be a place where you can find these answers without the “medical-speak” that makes everything sound scarier than it is. Trust your body, talk openly with your midwife or OB-GYN, and don’t skip doses. Getting that infection cleared up is one of the best things you can do to ensure a smooth path toward your due date.
FAQ: Quick Answers for Mom-to-Be
No. Bacterial infections are stubborn. If you stop early, the strongest bacteria might survive and come back even worse. Finish the whole bottle!
Extensive studies involving thousands of pregnant women have shown no link between Metronidazole use and an increased risk of miscarriage.
Yes, though a small amount does pass into breast milk. It might make the milk taste a bit bitter to the baby, but it is not considered harmful.