It is middle-of-the-night misery that every pregnant woman knows well: you are exhausted, but you cannot sleep because your nose is completely blocked. Whether it is seasonal allergies or the dreaded “pregnancy rhinitis” caused by shifting hormones, the simple act of breathing becomes a chore. When you reach for that bottle of Flonase on your nightstand, you stop and wonder if it is truly safe for the little life growing inside you.
As a gynecologist who has spent years helping women navigate these exact worries, I can tell you that you are right to be cautious. Your body is different now, and how it handles medication has changed. At PregnancyClarity, we aim to give you the straight facts so you can find relief without the stress.
The Short Answer: Can You Use Flonase While Pregnant?
If you are looking for a quick “yes” or “no,” the answer is generally yes, but with a few medical “ifs” and “buts.” Most OB-GYNs and allergy specialists consider Flonase (which contains the active ingredient fluticasone propionate) to be a low-risk option during pregnancy.
The reason doctors often feel comfortable with nasal sprays is because of something called “low systemic absorption.” When you swallow a pill, the medicine goes through your digestive tract and into your bloodstream, which eventually reaches the placenta. However, when you spray a fine mist like Flonase into your nose, the vast majority of that medicine stays right there in your nasal tissues. Only a tiny, negligible amount ever makes it into your blood.
Understanding the FDA Safety Ratings
In the past, the FDA used a letter-grading system (A, B, C, D, X) to rank drug safety. Flonase was traditionally placed in “Category C.” This often sounds scarier than it is. Category C simply means that there haven’t been large-scale, controlled clinical trials on pregnant women, largely because it is ethically difficult to test new drugs on expectant mothers.
Instead, we rely on “real-world evidence.” Because millions of women have used fluticasone while pregnant over the last few decades, we have a wealth of data. So far, this data does not show a clear link between normal doses of Flonase and birth defects or pregnancy complications.
The First Trimester Threshold
As a doctor, I usually advise my patients to be extra careful during the first twelve weeks. This is the period of organogenesis, where the baby’s heart, lungs, and limbs are forming. If your allergies are manageable, I often suggest sticking to drug-free options until you hit the second trimester.
However, if your symptoms are so severe that you cannot sleep or eat, or if they are triggering asthma attacks, the risk of “uncontrolled symptoms” might be higher than the tiny risk of the medication. If nasal sprays don’t provide enough relief, many doctors find that is Zyrtec safe during pregnancy as a second-line oral option to help you get through the day.
Why Your Nose is So Stuffy Right Now
It isn’t always pollen or pet dander. Many of my patients suffer from “pregnancy rhinitis.” When you are pregnant, your blood volume increases by about 50%. This extra blood flow causes the delicate membranes inside your nose to swell. High levels of estrogen also contribute to mucus production.
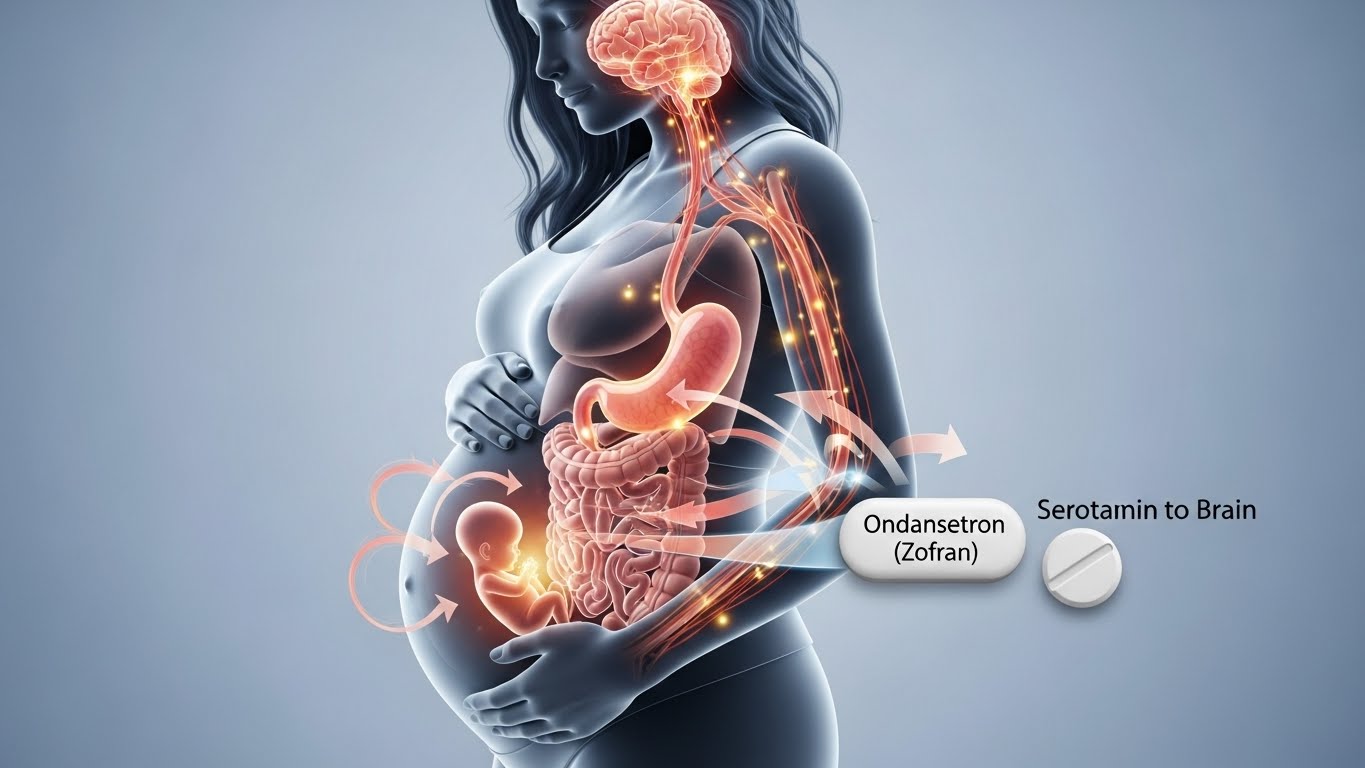
Much like how is zofran safe during pregnancy is a common question for morning sickness, Flonase is the go-to for these nasal issues. If your congestion feels like a constant cold that never ends, it is likely hormonal. Flonase works by reducing that inflammation, helping those swollen tissues shrink back down so air can actually pass through.
How to Use Flonase Safely
To keep the amount of medicine in your system as low as possible, technique matters. Here are my tips for using it correctly:
- Clear the Path: Use a simple saline spray first to wash out any crust or mucus. This helps the Flonase reach the tissue instead of just sitting on top of the gunk.
- Aim Away: Don’t spray straight up or toward the middle of your nose (the septum). Instead, point the nozzle slightly toward the outside of your nostril, toward your ear. This prevents nosebleeds and irritation.
- The “Stay Low” Rule: Always use the lowest dose that keeps you comfortable. For many women, one spray in each nostril once a day is enough to keep the swelling down.
Comparing Flonase to Other Options
Not all nasal sprays are created equal. If you are nervous about Flonase, you might hear about Rhinocort (budesonide). For a long time, Rhinocort was the only nasal steroid with a “Category B” rating, making it the “preferred” choice for many old-school doctors.
However, recent studies have shown that fluticasone (Flonase) and budesonide (Rhinocort) have very similar safety profiles. If Flonase is what you have in your cabinet and it works for you, most modern practitioners will tell you to stay the course.
Drug-Free Alternatives to Try First
I always encourage my patients at PregnancyClarity to try the “natural route” before reaching for steroids. These can be surprisingly effective:
- Saline Irrigation: A Neti pot or a NeilMed sinus rinse is your best friend. It physically flushes out allergens and thins the mucus without any drugs at all.
- Elevation: Sleep with an extra pillow. Gravity is a simple way to keep fluid from pooling in your nasal passages at night.
- Hydration: Drinking plenty of water keeps your mucus thin. If you get dehydrated, that mucus becomes thick and “glued” to your nasal walls.
- Steam: A warm shower before bed or a humidifier in the bedroom can provide temporary relief by moisturizing the dry membranes.
When to Be Concerned
While a stuffed nose is a nuisance, it is rarely a medical emergency. You should, however, call your doctor if:
- Your mucus is thick and yellow or green (which might mean a sinus infection).
- You have a high fever or facial pain.
- You have frequent nosebleeds that won’t stop.
- Your breathing issues are making it hard to catch your breath or causing chest tightness.
If you are still in the “two-week wait” and worried about early exposure before a positive test, check our guide on how soon can you take a pregnancy test to get an accurate result quickly and ease your mind.
Common Questions from My Patients
Sensimist uses a different type of fluticasone (furoate), but the safety profile is almost identical to the original formula. Many women prefer it because it has no scent and no “drip” down the back of the throat, which can be a lifesaver if you are already dealing with nausea.
Yes. The amount that makes it into your bloodstream is tiny, and the amount that would make it into breast milk is even smaller. It is considered very safe for nursing mothers.
Unlike oral decongestants (like Sudafed), Flonase does not typically raise blood pressure. This makes it a much safer choice for women who are at risk for gestational hypertension or preeclampsia.
Final Thoughts for the Expectant Mother
Being pregnant means making a thousand tiny decisions every day to protect your baby. It is exhausting, and it is okay to want to feel better. Congestion isn’t just a minor annoyance; it affects your sleep, your mood, and your energy levels.
When used as directed and preferably after the first trimester, Flonase is a helpful tool that many doctors trust. Always have a quick chat with your own OB-GYN or midwife before starting any new routine, as they know your specific health history best. For more honest advice on navigating these nine months, keep exploring PregnancyClarity. We are here to help you breathe a little easier.